In matters of risks and side-effects …
| 10. Mai 2017Patients who take medications often simply accept the potential side-effects. Only few people realize that such side-effects can be lethal. The pharmacist Gerhard Ecker and his team are developing computer models that can reliably detect the side-effects of substances at an early stage.
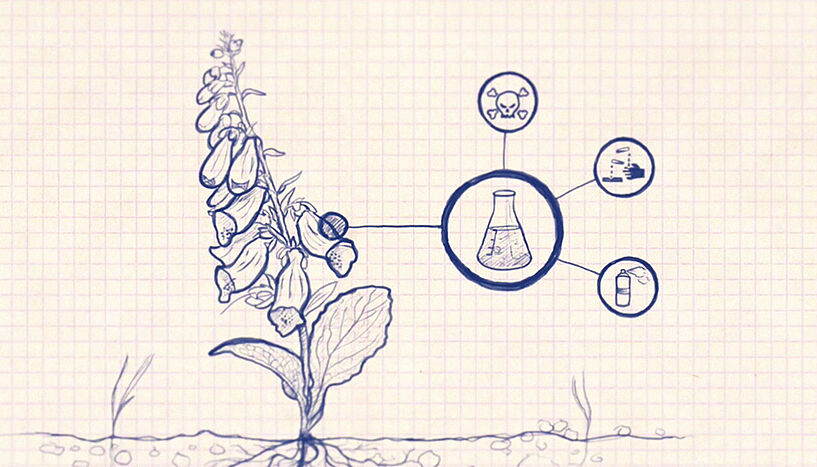
Patients who take medications often simply accept the potential side-effects. Only few people realize that such side-effects can be lethal. The pharmacist Gerhard Ecker and his team are developing computer models that can reliably detect the side-effects of substances at an early stage.
7000 persons in Austria die every year due to drug-drug interactions. In the US, this is the fourth most common cause of death. "Taking five to six medications simultaneously harbors an 80% chance of severe side-effects," says Gerhard Ecker from the Department of Pharmaceutical Chemistry.
Such "medication cocktails" are not the only risk. Even taking a single medication can trigger lethal side-effects. According to the expert, "The biological system is so complex that it is not possible to state with certainty whether – and where in our bodies – a particular molecule might trigger a negative effect."
Complex interplay
This should all change in the future: In order to detect potential side-effects at the earliest possible stage, Ecker and his team – in the framework of the major EU project TransQST – is developing computer models that depict the complex interplay of protein networks and thereby predict side-effects: "We are dealing with complex types of toxicity and therefore need to view organisms and cells holistically." In this effort, his research group is concentrating on "data mining" and "data integration": In the framework of the recently completed EU project OpenPHACTS, his team gained a wealth of expertise and has established itself as a leading expert group.
uni:view: We would be interested in hearing your answer to our current question of the semester: "Health from the lab – what is possible?"
Gerhard Ecker: Individualized drug therapies is the new buzzword and will take us a major step forward. This refers to the administration of individualized medications for individual patients. My wife and I have already had our genetic finger prints determined: This allows us to determine which medications are broken down quicker or more slowly in our bodies and therefore how their doses need to be adjusted. In the future, this could for example be done directly at pharmacies. Such an improved "medication management" would also help reduce dangerous drug-drug interactions. Combining this with the individual genetic profile – and in a subsequent step with the human microbiome, along with ever more specifically designed molecules – will enable developing much more targeted therapies. Creating genetic profiles, however, is also a societal issue and we will have to participate in the ongoing discussions.
Side-effects with consequences
Whether and where side-effects turn up depends on the toxicity of a particular compound: "Classical toxicity is triggered by chemical reactivity, mutagenicity or teratogenicity," says the pharmacist. Translation please! "Genetic information is changed in the nucleus: such mutations can lead to tumors or, in pregnant women, to deformities in the children. Teratogenicity, in turn, refers to an impact on the germ line, damaging the embryo."
The most infamous example of the latter is the drug thalidomide and the so-called Contergan scandal it triggered in 1961. "Thalidomide was a teratogenic compound," explains Ecker. While such a substance couldn’t slip through modern testing procedures, even today many drugs that would be unable to pass current approval procedures are still on the market. "Acetylsalicylic acid (ASS, aspirin) – with its chemical reactivity and its side-effects on the stomach lining would have no chance of becoming a painkiller today," is an example that Ecker likes to cite.
Four organs bear the brunt
The gastrointestinal system, as the point of "first entry", is one of the four organs in the focus of the project TransQST. The other three: liver, kidney and heart. "Every substance must go through the liver. Here, chronic toxicity is the primary issue because it is particularly difficult to assess and cannot be simulated in the lab," the researcher from the University of Vienna emphasizes. Importantly, the expert continues, not only is the liver changed by substances, but the substances themselves are changed by the liver: "Drugs are metabolized in the liver, i.e. chemically altered, in order to prepare them for excretion." In some cases this process makes them even more reactive than in their original form: the very features we try to use in developing medications – i.e. designing them such that they first unfold their effect in the liver – sometimes makes them even more toxic.
Since everything exits our bodies via the kidneys, they are also prone to side-effects. In the heart, substances can "bind" to a particular ion channel, the "hERG canal," blocking it and triggering deadly heart rhythm disturbances. "The underlying problem: this hERG channel has a very unspecific detection pattern," says Ecker.
Using a combination of data mining and complex similarity algorithms, Gerhard Ecker has developed a system that will make this toxicological "cross-reading" considerably more efficient in the future. "Based on the experience that we have gained in the framework of OpenPHACTS and eTOX, a precursor project of TransQST, we can recognize the problems in practice and have accumulated the necessary expertise to tackle them," says Ecker proudly.
Algorithm recognizes dangerous substances
Although several good models are already available to detect classical toxicity, complex types of side-effects still remain unpredictable. "We are currently developing the first algorithms and predictive models that combine high precision with high sensitivity. For this approach we crunch large amounts of data on chemical compounds that are provided to us by pharmaceutical companies," is how the scientist describes the process. The goal is to identify solely those substances that are dangerous – with a degree of precision high enough to ensure that no such substance is ever overlooked. "This is an important step forward in minimizing the side-effects of future drugs," concludes Ecker.
Semester Question 2017: "Health from the lab – what is possible?"
The straighter path to effective medications
Toxicity and lack of effectiveness are the main reasons why many drugs fail to make it past the clinical studies, i.e. the last phase in the development of medications. "If reliable computer models were already available in the early phase, the developers would need fewer resources – and much less animal testing would be necessary," the scientist explains. After all, it costs somewhere between one and ten million Euros to test a substance in experiments with animals. The total price tag until a drug finally comes on the market? About two billion Euros! This is money that Ecker feels could be saved in the future: "Using our models would enable us to concentrate only on the "safe" substances right from the very beginning, helping to reach the goal much more quickly and efficiently." (Text: Petra Schiefer, Translation: Mischa Stachowitsch)
The EU project transQST "Translational quantitative systems toxicology to improve the understanding of the safety of medicines" in the framework of the Innovative Medicines Initiative (IMI) extends from 1.1.2017 to 31.12.2021. Beyond the research team at the University of Vienna under the directorship of Univ.-Prof. Mag. Dr. Gerhard Ecker from the Department of Pharmaceutical Chemistry, this involves a cooperation with 20 other European universities, research facilities and pharmaceutical companies.